I recently reviewed two calls for one of our client agencies. Both call were responded to by the same two medics. Both patients were similar in some regards and the mistakes made were very similar.
Here is some of the relevant report, with Protected Health Information (PHI) removed or changed. Note that I’m not using the built in quotation function on the blogging platform, but you’ll be able to identify the text.
Here is the first report.
A3 dispatched to above address for a 68 year old pt not feeling well. Upon our arrival found a 68 y/o male ambulatory outside of him home with crew of FD. Pt was in no obvious signs of pain or distress. Pt stated his stomach has not felt right for the past x2 days. Pt denied any recent illnesses/injuries/surgeries. Pt denied any change in eating habits and states he has been drinking fluids appropriately. Pt had no other stated complaints. PMHx, Meds and allergies as noted.
Past Medical History: Hypertension
Medications: Aspirin Metoprolol
Allergies: None Known
The vital signs were,
BP 158/72
Mean Arterial Pressure 101
Heart Rate 78,
Pulse Ox 97
Respiratory Rate 16
Exam was not remarkable, including the abdominal exam.
Treatment consisted mostly of a ride to a nearby community hospital.
What, you may ask did they do incorrectly? That’s a qood question because on the surface this seems pretty straight forward, but it’s not. While typically EMS providers are taught that Acute Cardiac Syndrome (ACS) presents with chest pain or discomfort, that’s not always the case. A good percentage of cardiac patients have “atypical” complaints and that’s where experience and looking past the obvious differentiates a clinician from a technician. In this case as soon as I read a sort of vague abdominal discomfort I immediately looked for the attached 12 lead EKG. The problem being that there wasn’t one. Epigastric discomfort is a common atypical presentation of ACS. It’s usually associated with either a Myocardial infarction or Angina effecting the right side of the heart.
So, the first mistake was not looking past the obvious. This is not some sort of secret in medicine. Epigastric distress is right there in their protocols along with several other things that for years were just not recognized. So, this gentleman with a not very complicated medical history is possibly having a serious cardiac issue. IF it were recognized by the crew it could have been treated. That said you don’t treat what you don’t recognize.
As baseball great Yogi Berra said, “You can observe a lot by watching.” People joked about a lot of things he said, but this one was spot on. If you aren’t looking for something, you’ll never see it. In this case it would be reasonable to apply the stickies and hook up the cardiac monitor. A 12 lead EKG would have been interesting to look at, but alas they providers didn’t perform one. Nor did they place an IV line in case treatment was needed. Nor did the give the patient aspirin to chew.
Unfortunately for me and my readers I have no way to find out what happened to the patient. At least I know that he made it to the hospital alive.
Case number 2 involves the same crew. Which is not encouraging.
Herewith are the pertinent parts of their report. I apologize for the all caps narrative. Among other issues, this young lad can’t see to find the Caps Lock on his device,
“A3 D/P TO A/A FOR A 79 YOM REPORTED HYPERTENSION AND STOMACH DISCOMFORT. UOA TO SCENE PT WAS FOUND SITTING UPRIGHT IN CHAIR IN HOME STATING THAT ON AND OFF FOR THE PAST 12 HOURS
HE STARTS TO GET PAIN IN HIS STOMACH ACCOMPANIED WITH BILATERAL ARM WEAKNESS AND EXPERIENCING PAIN IN HIS JAW . PT STATES IT WOULD COME ON FOR 5-10 MINUTES AND THEN SUBSIDE.
PT WAS TAKING HIS OWN BLOOD PRESSURE AND STATES THAT IT WAS HIGH. PT STATES HE WAS SEEN THE WEEK PRIOR AT {nearby community hospital} FOR THE SAME ISSUE AND WAS DIAGNOSED WITH COPD BUT PT
DENIES SOB AT THIS TIME. PT ASSISTED TO STRETCHER SECURED AND TAKEN INTO A3 FOR FURTHER EVAL/TRANSPORT ”
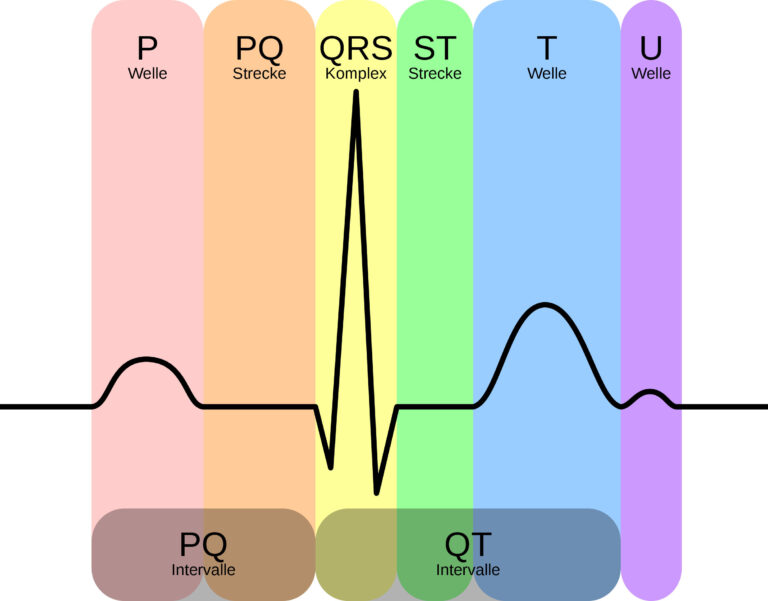
This one is a bit more slippery because they did obtain a 12 lead EKG. Nine of them to be exact, but some were not clear enough to read. The provided noted some ST Depression in Leads V4 and V5 (chest leads). The problem with that is that those are not contiguous despite the number. Also, when I read the EKG (and I’m much more experienced that the two medics combined) I noticed that actually the anomaly was present in four chest leads, not just two.
Note that this too is a complaint of abdominal pain, but along with that there is pain in his jaw and weakness in both of his arms. It would be helpful if the medic had said which side of the jaw, but that’s not particularly critical. Once I read that complaint I went looking for the EKG (found) IV (found) and the Aspirin (nope). For more than twenty years now Aspirin has been recognized as a critical component of treatment for chest pain. Not that it make the pain go away, but that it makes the blood cells a bit more slippery and reduces clotting of red blood cells.
In this case, for reasons not clear to me they bypassed three hospitals with emergency cardiac catheterization labs and drove about half an hour to a fourth. Fortunately for the patient and them, nothing bad happened. There was something going on, however even to me it isn’t clear exactly what.
Sometime something that appears simple is far from simple. There were times in my field career that I’d look at a patient and get a funny feeling in my stomach. “Gut instinct” we’re told it is, but I don’t know how my gut can tell that a patient is about to fall of a clip. I don’t know how it does, but it does. In both of these cases, I’d have had that feeling in my stomach and would have treated these patient more aggressively than they were inclined to.
Does this make me a super smart paramedic? No, just one that pays a lot of attention to subtle clues.